The 15th Finance Commission maintained states’ higher share of central taxes while recommending an overall increase in government health spending to prepare better for the next pandemic, but the increase is inadequate considering low health spending per capita, say public health experts.
The Covid-19 pandemic, and particularly its second wave, exposed serious deficiencies in the public health systems of several states. People struggled with shortages of hospital beds, supplies of oxygen, and other essential resources, we reported in April 2021.
Further, the pace of adding dedicated Covid-care facilities and oxygen-supported beds actually slowed between the first and second waves. Limited laboratory capacity led to compromised testing and questionable case detection, surveillance and outbreak management, all of which, the 15th Finance Commission reported, underlining the inadequacy of critical care infrastructure. These inadequacies occurred despite states receiving greater rights over funding under the 14th Finance Commission.
Finance commissions (FC) are constitutional bodies formed every five years to give suggestions on Centre-state financial relations, to make recommendations on sharing of central taxes, and to give central grants to states for the relevant five-year period.
The 15th FC report, tabled in Parliament on February 1, 2021, looked closely at the health sector, and fixed tax devolution from the Union government to the states at 41%, down from 42% during the 14th FC period to account for the creation of the Union territories of Jammu & Kashmir and Ladakh. It called on states to increase health spending to a minimum of 8% of their total spend by 2022.
The 15th FC also called on the Union government to increase its health spending, recommending that public health expenditure of the Union government and the states combined should be increased progressively to reach 2.5% of the Gross Domestic Product (GDP) by 2025. These recommendations are for the period April 1, 2020 to March 31, 2026.
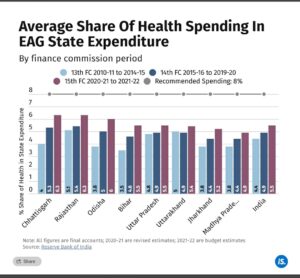
To understand why the 15th FC focussed on the health sector, we look at the health spending of eight Empowered Action Group (EAG) states during the 14th FC period. The eight EAG states–Bihar, Jharkhand, Uttar Pradesh, Uttarakhand, Madhya Pradesh, Chhattisgarh, Odisha and Rajasthan–account for about 47% of India’s population; they are more rural and socioeconomically backward compared to the rest of the country.
They are also high focus states under the National Rural Health Mission (NRHM), in view of their relatively higher fertility and mortality indicators. Bihar, Jharkhand, Madhya Pradesh and Uttar Pradesh are among India’s five poorest states.
India Spend reached out to the principal secretaries for health and finance of all EAG states, and the joint health secretary and economic advisor in the Union government. This story will be updated when we receive a response.
Health spending increase during the 14th FC
A portion of central taxes, such as customs duty, income tax, service tax and central excise duty, are transferred to states as untied funds, which states can spend according to their discretion.
The 14th FC increased the devolution of taxes from the Union government to states from the erstwhile 32% to 42% to give states greater flexibility and autonomy in their spending on state subjects including health.
During the period of the 14th FC, the average annual transfers of funds from the Union government nearly, or more than, doubled for all EAG states except Uttarakhand. These higher transfers were maintained during the first two years of the 15th FC period as well (See chart).
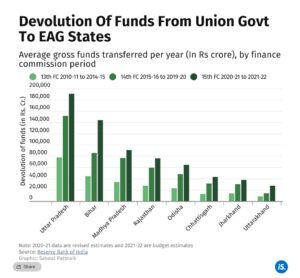 “The 14th Finance Commission, among other recommendations, had put the onus of social sector spending a lot more on states,” Simonti Chakraborty, senior programme officer at the Centre for Budget and Governance Accountability, a Delhi-based think-tank, told India Spend. “The idea was that with the increase in availability of funds, the onus of spending on social sector schemes, including public health, should be more on states.”
“The 14th Finance Commission, among other recommendations, had put the onus of social sector spending a lot more on states,” Simonti Chakraborty, senior programme officer at the Centre for Budget and Governance Accountability, a Delhi-based think-tank, told India Spend. “The idea was that with the increase in availability of funds, the onus of spending on social sector schemes, including public health, should be more on states.”
It is therefore pertinent to see if the increased devolution to states–particularly the EAG states–resulted in a corresponding increase in health spends.
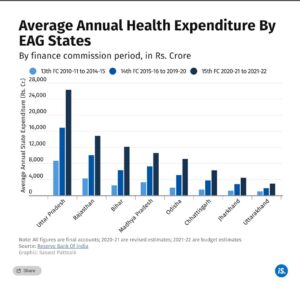
Health spending during the 14th FC period nearly or more than doubled in all states except Uttarakhand, compared to the 13th FC period. Further, those expenditures increased even further in the first two years of the 15th FC period.
When you drill down further, as with the chart above, you notice that though the EAG states spent more on health during the relevant period, they still fell short of the 15th FC’s recommendation of a minimum 8% of total spending, as of November 2021. Note also that Jharkhand and Madhya Pradesh have, over the last 12 years, spent less than the Indian average on health as a percentage of total spend.
Uttarakhand made the lowest increases in health spending among all EAG states during the 14th FC period, but the state’s base health performance is better than the other seven states on most metrics, per Ministry of Health and Family Welfare (MoHFW) data. Uttarakhand outperformed the Indian average on multiple indicators during the 14th FC period, per consecutive National Family Health Survey (NFHS) reports.
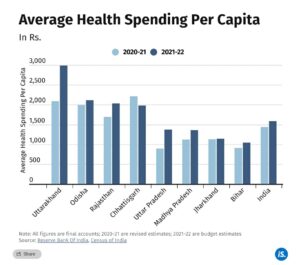
Drill down further into the data (see chart below), and you find that Uttarakhand spent more on health per capita than the other EAG states or even the countywide average during the first two years of the 15th FC. Chhattisgarh, Odisha and Rajasthan also spent more than the India average, while Bihar, Jharkhand, Madhya Pradesh and Uttar Pradesh spent less.
Why focus on increased health spending?
The 15th FC’s sharp focus on healthcare spending stems from the realisation that health infrastructure in the EAG states is inadequate. Our analysis shows that at the end of the 14th FC period, there were significant shortfalls in both physical infrastructure, such as primary health centres, and in manpower–doctors and paramedic staff–which is the biggest area of state health expenditure.
The 15th FC report highlighted a “severe deficit of public health facilities” in Bihar, Jharkhand and Uttar Pradesh (and West Bengal, among the non-EAG states). All three EAG states lag behind the Indian average of rural population per health centre. Madhya Pradesh did improve significantly on this metric during the 14th FC period, but still lags behind the national average.
One possible explanation is that the result of increased healthcare spend is not immediately visible on the ground. “Health impacts have a longer gestation period,” former Union Health Secretary J.V.R. Prasada Rao told IndiaSpend. “It’s not like building 100,000 toilets, which is measurable, because next year you can see how many toilets have been built. Any improvement in the health status of people is normally measured with a gap of 3-4 years by the National Family Health Survey.”
Where do EAG states come up short?
The biggest line item in healthcare spending by states is manpower–and in this area, the performance of EAG states is sub-optimal, as seen in the deep dive below.
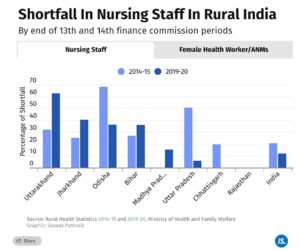
The smallest shortfalls in rural health manpower in all eight EAG states are among lower rung workers (see chart above), including female health workers and auxiliary nurse midwives (ANMs).
Shortfall in rural nursing staff increased in four of the eight EAG states–Bihar, Jharkhand, Madhya Pradesh and Uttarakhand–at the end of the 14th FC period.
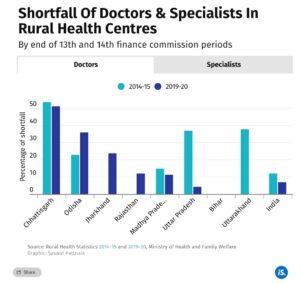
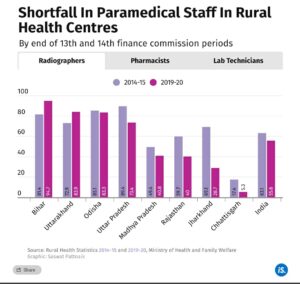
Moving up the rungs of the rural health workforce, manpower shortfalls in paramedical staff, doctors and specialists improved in some EAG states during the 14th FC, compared to the previous five years, but gaps remain significant in many states (see chart).
Chhattisgarh, Madhya Pradesh, Jharkhand, Odisha and Rajasthan have significant shortfalls in the number of doctors at rural health centres, though the first two states managed to slightly reduce the gap during the 14th FC period. Uttar Pradesh and Uttarakhand made significant progress on this metric.
Despite an improvement, the data show that three in four specialists were missing from India’s rural health centres at the end of the 14th FC period. The number is as high as nine in 10 missing specialists in Chhattisgarh and Madhya Pradesh.
Further, among paramedical staff, one in two radiographers, one in five pharmacists, and one in three laboratory technicians are missing from India’s rural health workforce, and the shortfalls in several EAG states are larger than the national figures.
The worst performer is Bihar, with a 95% shortfall of radiographers, 72% shortfall of pharmacists and 75% shortfall of lab technicians at rural health centres by the end of the 14th FC period.
Causes and consequences
Experts suggest a dependence on contract labour, reluctance by states to spend money on long term health goals, lack of proper budgeting, and the reluctance of doctors to take up government jobs among the factors behind the chronic manpower shortfall.
“I think doctors–or any other human resources–are seen as a financial liability by governments, because if you appoint somebody, then the government has to pay for them all the way up to his or her pension,” Rakhal Gaitonde, professor of public health at the Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvananthapuram, told IndiaSpend. “This is the reason for an increased shift towards contract labour.”
Contractual labour however is not sustainable as it affects the stable functioning of the public health systems, said Ravi Duggal, health researcher and activist, associated with the People’s Health Movement, a global network of grassroots health activists. “If you have a doctor coming in for a year, and then another doctor coming in for the next year, the doctor will not be interested in working. When the state is not committed to the doctor, doctors will not make commitments to the public health system.”
The rising cost of medical education is a contributing factor. Several Indian medical students who were recently evacuated from Ukraine after Russia invaded the country on February 24, 2022 said it was cheaper for them to study there, as the cost of medical education in India was prohibitive. Others said there weren’t enough seats available in medical colleges in India.
The 15th FC report highlighted this shortage and pointed to the asymmetric distribution of medical colleges, with most located in the western and southern states. The 15th FC called for specialist medical courses to be conducted at all public health facilities, and for annual recruitment of doctors based on state-wise needs.
“Medical education is expensive, with students spending anything between Rs 5 to 10 million (Rs 50 lakh to Rs 1 crore) for an MBBS degree,” pointed out Indranil Mukhopadhyay, associate professor at Jindal Global University. “Doctors want to earn, so they go to the private sector, and many states are finding it difficult to get doctors for rural health centres.”
Lack of staff leading to closure of sub-centres
A domino effect comes into play in the given set of circumstances: States spend less on professional healthcare specialists, therefore such specialists are unwilling to work for the government, and therefore there are critical personnel shortfalls in the healthcare ecosystem. And this shortfall in doctors and nursing staff, in turn, led to the shutting down of health centres.
The 15th FC report points out that primary healthcare in rural areas is provided via sub centres linked to primary (PHC) and community (CHC) health centres, and highlights “significant shortfalls” in PHCs and CHCs and a “severe deficit of public health facilities” in Bihar, Jharkhand, Uttar Pradesh and West Bengal. The newly announced Health and Wellness Centre (HWCs), which offer a range of services spanning preventive, promotive, curative, rehabilitative and palliative care for all ages, would put more pressure on the already stressed manpower.
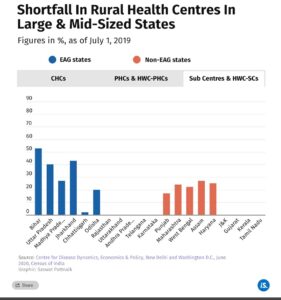
Towards the end of the 14th FC period, six months before the first Covid-19 case was detected in India, Bihar, Jharkhand, Uttar Pradesh and Madhya Pradesh had the largest shortfalls in rural health centres among all large and mid-size states with a population of 10 million and above, the MoHFW informed Parliament on March 12, 2021.
“The (Union) minister himself has gone on record saying that there’s a 23% fall in PHCs and sub centres too,” Union Health Secretary Prasada Rao points out. “This is mainly because of the lack of adequate number of ANMs to manage the centres. State health departments are not taking care to see that the sub centres sanctioned actually function in the field.”
This is borne out by the chart below, which shows that among EAG states, only Rajasthan and Uttarakhand had no shortfall in rural health centres before the Covid-19 pandemic struck. Chhattisgarh and Odisha had smaller shortfalls in such centres, compared to the countrywide average.
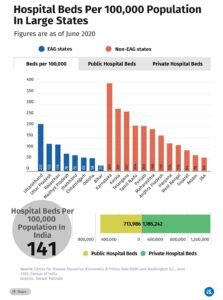
Besides personnel, another lens to look at the issue is by examining the number of available beds per 100,000 people. On this measure, Bihar is the worst performer, with just 25 beds per 100,000 people as of 2020, against the national average of 141 beds. Compare that with the best performer among non-EAG states–Karnataka, which has 395 beds per 100,000 people. Among the EAG states, only Uttarakhand has more hospital beds than the Indian average.
The domino effect, and the reasons why
Shortfall in PHCs, in trained personnel, in hospital beds particularly in rural areas–it all adds up. “Healthcare,” says Duggal, “is a labour-intensive sector, with health staff providing everything from counselling to surgery to post-op care. So 70-80% of state expenses going towards salaries is to be expected. However, this should not mean that the need for building more health facilities can be ignored.
“There is a need to benchmark money for salaries while drawing up the budget, and also to benchmark money for non-salaries as well. This helps the government ensure that it does not overspend on either staff or health centres.”
Experts also point out that often, money allocated does not equal money received. “It costs close to Rs 4-5 million (Rs 40-50 lakh) to run a fully functioning PHC, given that it requires a staff strength of two doctors, several ANMs and other paramedics, plus medicines etc.–but in reality, only Rs 1.5-2 million (Rs 15-20 lakh) is allocated,” Duggal points out. “There will therefore be vacant positions, short supply of medicines, poor maintenance leading to leaky roofs and filthy toilets. States with a resource crunch argue that there is no point in running such centres–it is seen as wasted expenditure, because it’s not serving the purpose.”
Impact on women and children
The 15th FC report had noted that despite improvements, India continues to lag behind similarly-placed countries on key health outcomes related to child and maternal health, including infant and maternal mortality rates, nutritional outcomes and rate of institutional deliveries.
Nutritional outcomes among children, the 15th FC report noted, have long-term implications not only for their health but also for learning, employability and economic performance, and is a “development challenge of first-order importance”.
Stunting (low height for age), underweight (low weight for age) and anaemia levels in children hinder the development of primary immunity, the report noted. The Covid-19 pandemic has magnified the disparities, with lasting adverse effects on maternal and child health, particularly among the poor.
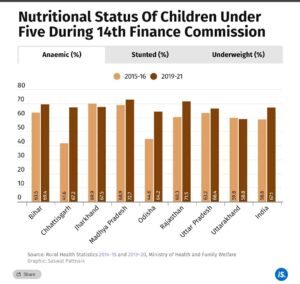
Two NFHS rounds, in 2015-16 and 2019-21, covering the start and end of the 14th FC period, indicate that all eight EAG states have improved in terms of childhood stunting, as also in underweight and anaemic children.
All EAG states have reduced childhood stunting at a greater rate than the Indian average. Bihar, Jharkhand and Uttar Pradesh, however, still have high levels of childhood stunting compared to the countrywide average. Bihar and Jharkhand also have high levels of underweight children.
Jharkhand and Uttarakhand have reduced levels of anaemia in children over the period covered, at a time when anaemia in children has increased significantly countrywide. The increase was sharper in Chhattisgarh, Odisha and Rajasthan.
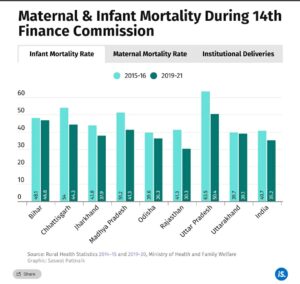
The 15th FC also pointed to disparities in the progress of states towards achieving the United Nations Sustainable Development Goal on maternal and child mortality rates, which aims at reducing infant mortality to 12 per 1,000 live births by 2030.
Infant mortality rates (IMR) per 1,000 live births fell in all EAG states during the 14th FC period, but still remained way above the numbers required to meet the UN SDG targets.
Again, the UN SDG target for maternal mortality is 70 deaths per 100,000 live births by 2030, against which India’s current maternal mortality ratio (MMR) is 130, according to the MoHFW. During the 14th FC period, all EAG states except Uttarakhand and Jharkhand had a higher MMR than the national average.
The 15th FC report outlined a higher number of institutional deliveries as a key health outcome. Institutional, or supervised, births had risen to nearly nine out of 10 births countrywide during the 14th FC period, NFHS data show. All EAG states have made significant progress on this metric; however, one in four births in Bihar and Jharkhand remained unsupervised by 2021.
“Infant mortality and maternal mortality has been a priority in public health,” said Avani Kapur, who leads the Accountability Initiative at the non-profit Centre for Policy Research. “But to ensure progress on maternal and child health, a critical aspect is improvement in access to good quality public health, whether in ensuring safe delivery or in receiving regular antenatal care.”
Data from Rural Health Statistics, Kapur points out, found that as of March 2020, only 72% of PHCs had a labour room, and that there is a shortfall of 69.7% obstetricians and gynaecologists, and 78.2% paediatricians. “This can have an impact on India’s progress towards meeting its IMR and MMR goals.”
“The political leadership in these northern states have not put adequate priority on people: on people’s education, people’s health, people’s housing, etc.,” Prasada Rao points out. “That is why you find that perennially, in these states, people suffer because of these low social indicators.”
Prachi has two masters degrees: In economics from Mumbai University and in development studies from the University of Sussex, UK. She holds a bachelor’s degree in economics from St. Xaviers College, Mumbai. She has been a research assistant at the Institute of Development Studies (UK) and the Young Foundation (UK). She has also worked for Greenpeace India in the fundraising division.
This article is published as a part of the Smitu Kothari Fellowship of the Centre for Financial Accountability, Delhi.
The original article published in IndiaSpend can be accessed here.
Centre for Financial Accountability is now on Telegram. Click here to join our Telegram channel and stay tuned to the latest updates and insights on the economy and finance.